The paper underscores the need for coordinated responses to promote mental wellness and resilience during the COVID-19 crisis.
Just like the rest of the world, the Philippines has also been seeing a rise in mental health concerns since the enhanced community quarantine (ECQ) was implemented in the entire Luzon in mid-March.
Calls for help
According to Dr. Roland Cortez, director of the National Center for Mental Health (NCMH), the number of calls being received by the NCMH Crisis Hotline has more than doubled since the ECQ started. This prompted the hospital to increase their hotline numbers from two to six
“Because of the uncertainty of the future, many people are calling us for help because they are very bothered with what is happening now. They have depression and anxiety,” he told THE STAR.
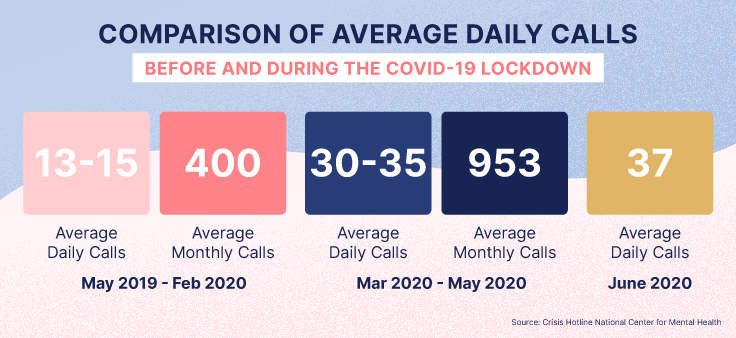
Data from the 24/7 NCMH Crisis Hotline showed from May 2019 to Feb. 2020, some 13 to 15 and 400 calls were received daily and monthly, respectively. This jacked up to 30 to 35 and 953 daily and monthly, respectively, from March to May 2020.
From March 17 to May 31, a total of 2,298 calls were received and these mostly involved health and financial concerns as the end of the pandemic is still nowhere in sight.
Cortez said callers were mostly worried that they and their loved ones would contract the virus. Because of this, even slight fever and cough can cause them to panic, thinking that they are already infected.
“They are also so afraid they have no work to go back to after the lockdowns. Others were already having financial problems because of the stoppage of work or their business,” he noted.
Before COVID-19, most callers had problems about squabbles and misunderstanding in the family, lovers’ quarrels or break-ups and having flunked an examination
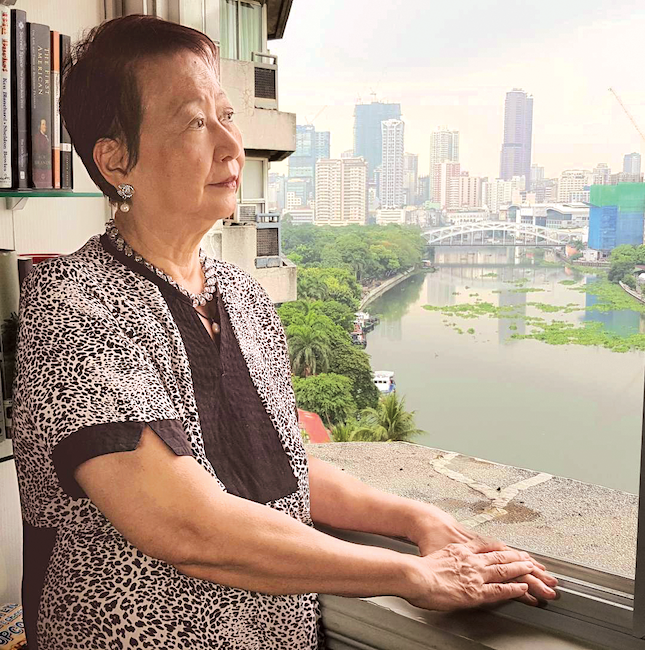
The elderly
The Natasha Goulbourn Foundation (NGF) has observed a 220-percent increase in callers to its 24/7 hotline HOPEline every day in the past four months and many of the callers are elderly.
NGF founder Jean Goulbourn said each day, there are some 72 to 138 calls and half of them are related to “COVID-19 lockdown and mortality.”
“We’re dealing with different age groups but interestingly, we never had such a big age group of seniors calling us. Right now, we have about 32 percent seniors calling, and they are locked in a condo-apartment,” she added.
Goulbourn had appealed to the public to spare time for their elderly who get depressed and anxious because of fear of the virus and the uncertain future of their families.
“It’s shocking that about 25 to 30 percent of our callers are widows who live alone…It’s just about being mindful of our relatives. If they don’t live with you, call them more often,” she said.
Survivor's tale
One of those lucky enough to survive COVID-19 is Health Assistant Secretary Charade Mercado Grande, 37, who admitted she would have had anxiety attacks while undergoing management and treatment in a hospital, if not for the “strong support” of her family.
“When you are alone in an isolation room and the fear of the unknown, and you don’t know if you will survive, it will really stress you. It’s good that I have strong family support and my friends are supportive. This helped me survive,” she said.
When told that she was infected with COVID-19 on March 30, Grande’s first thought was her family, especially her six-year old son, and the people she came in contact with. She did not expect that her illness would bring her family closer.
Although they were not physically together, Grande narrated that she, her husband and son prayed at the same time every day before going to sleep through video conferences.
And while she and her five siblings now have different religious beliefs, they communicated through Viber at 8 in the evening every day. They talked about GOD, their devotions and anything that they wanted to share with each other.
“I never imagined that we would be in one Viber group because we now have our own families and we live in different places… After I recovered, we continued with our communication and we would always check on each other,” she added.
Aside from this, her other “coping mechanisms” include listening to religious songs, watching inspirational movies and documentaries on YouTube and doing TikTok dances.
Self-awareness
For Dr. Nina Castillo-Carandang, a social health scientist from the University of the Philippines-College of Medicine, “self-awareness” of one’s mental condition is a key aspect in the search for well-being, happiness and health.
When exploring one’s mental health, she said it is important to recognize that “it’s okay not to be okay.”
“If we are prepared to share what we are going through with people that we trust like family and friends, we would realize that we are not alone and that many people love us,” she added.
Carandang added in this time of COVID-19, we can still be “socially connected but physically distant” through text messaging, social and traditional media, radio, TV, online religious services, among other platforms.
According to the World Health Organization, “the new realities of working from home, temporary unemployment, home-schooling of children, and lack of physical contact with other family members, friends and colleagues take time to get used to.”
These can be challenging especially for those who are already with mental health conditions but there are things that can be done to manage mental health.
These are:
- Be informed by following trusted news channels, such as local and national TV and radio, and keep up-to-date with the latest news from WHO on social media.
- Have daily routine that includes keeping up with personal hygiene, eating healthy meals at regular times, exercising regularly, allocating time for working and time for resting and by doing things you enjoy.
- Minimize newsfeeds.
- Maintain social contact through telephone and online channels.
- Avoid using alcohol and drugs as a way of dealing with fear, anxiety, boredom and social isolation.
- Limit screen time and make sure you take regular breaks from on-screen activities.
- Use social media to promote positive and hopeful stories.
- Help others.
(For more information, call the NCMH at 0917-899 USAP (8727) or 8989-USAP (8727); the Natsha Goulbourn Foundation’s 24/7 HOPELINE at (02) 8804-HOPE (4673),0917-558 HOPE (4673), and 2919 (toll-free number for all GLOBE and TM subscribers); the DOH COVID HOTLINE at 894 - COVID (26843); The UP College of Medicine at 8536-1368; and the WHO representative in the Philippines at 8528-9762.)